Introduction To Egg Freezing
In today’s evolving world, more and more women are choosing to delay motherhood for a variety of reasons — career advancement, personal growth, financial security, or not having met the right partner yet. With this shift, a significant question arises: what are my chances of getting pregnant after 35? And if I want to keep my options open, should I consider egg freezing?
This comprehensive guide will help you explore everything a woman over 35 needs to know about getting pregnant, late motherhood, and fertility preservation. We’ll cover the biology of aging eggs, the step-by-step egg freezing procedure, its pros and cons, associated costs, success rates, and most importantly — the emotional and psychological journey that accompanies these choices. Whether you’re considering egg freezing or natural conception, this detailed blog empowers you to make an informed decision.
1. Understanding Fertility Over 35
1.1 Biological Clock: What Changes After 35?
Women are born with about 1 to 2 million eggs, but by puberty, only around 300,000 remain. By the time a woman reaches 35, the number and quality of her eggs decline sharply — this is known as diminished ovarian reserve. Unlike men who continuously produce sperm, women’s egg count is finite.
Age-Related Changes in Female Fertility:
- Decline in Egg Quantity: Every menstrual cycle, multiple eggs begin to mature, but usually, only one ovulates. The others are lost. As age increases, fewer eggs respond to stimulation.
- Decrease in Egg Quality: Older eggs are more prone to chromosomal abnormalities. This raises the risk of miscarriages and genetic conditions like Down syndrome.
- Reduced Implantation Rates: Even if fertilization occurs, the chances of successful embryo implantation decrease with age.
- Increased Risk of Infertility: After 35, a woman’s chances of conceiving naturally decline steeply.
1.2 Natural Conception Success Rates by Age
| Age | Monthly Pregnancy Rate | Miscarriage Risk | IVF Success Rate |
|---|---|---|---|
| 30 | ~20% | ~10% | ~45% |
| 35 | ~15% | ~20% | ~35% |
| 40 | ~5-10% | ~33% | ~20% |
| 45 | <5% | >50% | ~5-10% |
Fertility clinics often recommend starting fertility assessment by 30 and freezing eggs ideally before 35 for best outcomes.
2. What is Egg Freezing?
2.1 Understanding Oocyte Cryopreservation
Egg freezing, medically called oocyte cryopreservation, is a breakthrough in fertility preservation technology. The procedure allows women to store their eggs when they are young and healthy, enabling a better chance at pregnancy later when natural fertility has declined.
It involves stimulating the ovaries to produce multiple eggs, retrieving them, and freezing them using a process called vitrification, which prevents ice crystal formation that can damage the egg’s structure.
2.2 Who Should Consider Egg Freezing?
Egg freezing isn’t just for women who want to delay motherhood. It is increasingly recommended for:
- Women undergoing chemotherapy or radiation therapy
- Women with polycystic ovarian syndrome (PCOS)
- Those with a family history of premature menopause
- Women who want to focus on career or education
- Women in their late 20s or early 30s who are single but want to plan for motherhood
By freezing eggs early, you retain the possibility of using younger, healthier eggs even if you try to conceive in your late 30s or 40s.
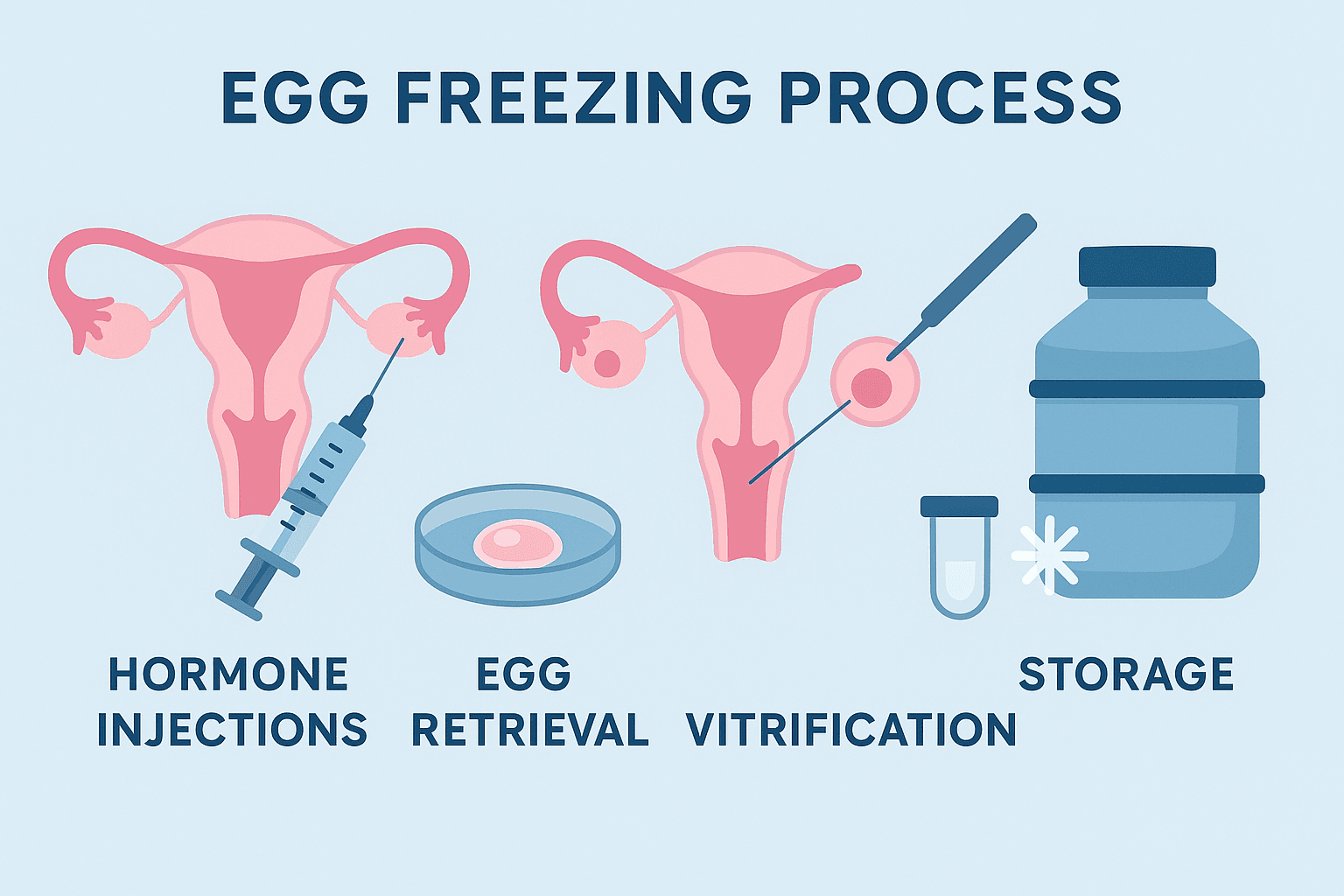
3. The Egg Freezing Procedure: Step-by-Step Guide
Understanding the procedure can ease fears and help you prepare mentally, physically, and emotionally. Here’s what to expect at each stage.
3.1 Step 1: Ovarian Reserve Testing
Before starting the procedure, your doctor will assess your fertility with the following tests:
- AMH (Anti-Mullerian Hormone) blood test
- Antral Follicle Count (AFC) via transvaginal ultrasound
- FSH (Follicle-Stimulating Hormone) levels
These tests help determine how many eggs are likely to be retrieved and your response to stimulation.
3.2 Step 2: Hormonal Stimulation
- Duration: 10 to 14 days
- Daily hormone injections (FSH and LH) to stimulate your ovaries to mature multiple eggs
- Frequent ultrasounds and blood tests to monitor growth and prevent overstimulation
Common hormone names: Gonal-F, Menopur, Cetrotide, Lupron
3.3 Step 3: Egg Retrieval (Oocyte Aspiration)
- Done under light sedation (not general anesthesia)
- A thin needle is inserted through the vaginal wall using ultrasound guidance
- The procedure takes about 20-30 minutes
- Recovery: Usually a few hours
3.4 Step 4: Vitrification (Freezing the Eggs)
- Only mature eggs are selected for freezing
- Rapid freezing prevents damage from ice crystals
- Eggs are stored in liquid nitrogen at -196°C
3.5 Step 5: Storage and Future Use
- Eggs can be safely stored for 10 years or longer depending on local regulations
- When ready, the eggs are thawed, fertilized via ICSI (Intracytoplasmic Sperm Injection), and the embryo is implanted in the uterus
This whole process is typically done at fertility centers under specialized care.
4. Risks and Side Effects of Egg Freezing
While egg freezing is generally safe, it’s important to be aware of the potential side effects and complications that may arise.
4.1 Short-Term Side Effects
These are usually mild and resolve on their own:
- Bloating and Abdominal Pain: Hormonal stimulation can enlarge the ovaries.
- Mood Swings: Due to elevated hormone levels.
- Breast Tenderness and Fatigue
- Bruising or Redness at Injection Sites
- Mild Cramping Post-Retrieval
4.2 Ovarian Hyperstimulation Syndrome (OHSS)
In rare cases, women may experience OHSS, where ovaries swell and leak fluid into the body. Symptoms include:
- Rapid weight gain
- Severe abdominal pain
- Shortness of breath
- Nausea or vomiting
Most OHSS cases are mild, but severe forms may require hospitalization.
4.3 Long-Term Considerations
- Emotional Risk: Many women place emotional hope in their frozen eggs. While empowering, it can also be anxiety-inducing.
- Financial Burden: The cost of the procedure, storage, and IVF can add up to several lakhs.
- Not a Guaranteed Pregnancy: Freezing eggs does not ensure a future baby. Success depends on age at freezing and egg quality.
- Ethical Dilemmas: If eggs are unused, some women face ethical questions about disposal or donation.
5. Late Pregnancy and IVF Outcomes Over 35
As more women choose to start families later in life, it’s crucial to understand the realities, both medical and emotional, of pregnancy after 35. While it’s absolutely possible to have a healthy baby, the journey may come with a few extra considerations.
5.1 IVF Success Rates Over 35
In-vitro fertilization (IVF) is a common fertility solution for women in their late 30s and early 40s. However, success rates vary based on age and egg quality:
| Age Group | IVF Success Rate per Cycle |
| Under 35 | 40-45% |
| 35-37 | 30-35% |
| 38-40 | 20-25% |
| 41-42 | 10-15% |
| Over 43 | <5% (with own eggs) |
Using frozen eggs from your early 30s can significantly increase the chances of success later, as those eggs are of better quality compared to freshly retrieved ones at older ages.
5.2 Physical Health Considerations in Pregnancy Over 35
Pregnancy after 35 is considered “advanced maternal age,” a clinical term that often triggers more frequent monitoring. Common risks include:
- Gestational diabetes: Hormonal changes affect insulin sensitivity.
- High blood pressure or preeclampsia: Can affect placental blood flow.
- Preterm birth or low birth weight: More common in older mothers.
- Placenta previa or placental abruption: Related to uterine lining conditions.
- Higher chance of cesarean section
- Chromosomal abnormalities in the baby, such as Down syndrome
Because of these, regular prenatal checkups and diagnostic screenings like non-invasive prenatal testing (NIPT), nuchal translucency scans, and amniocentesis are recommended.
5.3 Lifestyle Recommendations to Support Pregnancy
The quality of your lifestyle can make a major difference when trying to conceive and during pregnancy. Here are proactive steps to increase your chances of a healthy pregnancy:
- Maintain a balanced, nutrient-dense diet rich in folate, iron, and omega-3s
- Stay physically active with low-impact exercises like walking, swimming, or prenatal yoga
- Avoid alcohol, tobacco, and excessive caffeine
- Get enough sleep and manage stress levels through mindfulness practices
- Consult with a fertility nutritionist to optimize preconception health
These habits not only support conception but also foster a healthier pregnancy environment for both mother and baby.
5.4 Emotional Readiness for Motherhood After 35
Many women over 35 report feeling more emotionally prepared for parenthood — they have a better sense of self, financial stability, and relationship clarity. However, concerns often arise, such as:
- Will I have enough energy to raise a child?
- What if I need medical help to conceive?
- How will society or family perceive a later-age pregnancy?
Supportive counseling or parent communities can help ease these anxieties and normalize the evolving timeline of modern motherhood.
6. Emotional and Psychological Impact of Fertility Preservation and Late Pregnancy
While medical procedures like egg freezing and IVF come with clinical instructions and protocols, the emotional and psychological journey is deeply personal — and often less talked about.
6.1 Emotional Reactions to Egg Freezing
Women often feel a range of emotions before, during, and after the egg freezing process:
- Empowerment and Relief: Many feel empowered by taking control of their reproductive future. Egg freezing can offer peace of mind.
- Anxiety and Fear: What if the eggs don’t survive the thaw? What if it doesn’t work when I need it?
- Hope vs. Pressure: The phrase “insurance policy” is often used to describe frozen eggs, but this can lead to performance pressure later in life.
- Loneliness: This decision is often made alone. Emotional support from friends or a therapist can help.
6.2 The Psychological Weight of Delayed Motherhood
For women trying to conceive later in life, emotions may include:
- Frustration: Failed cycles or delayed results can feel demoralizing.
- Comparison: Seeing younger women conceive easily may spark feelings of inadequacy.
- Regret or Guilt: Some may wonder if they waited too long.
- Fear of Judgment: Society often still views motherhood through a narrow age lens.
6.3 Coping Mechanisms
Navigating these complex emotions requires proactive support:
- Therapy or Fertility Counseling: Especially helpful to manage expectations and reduce anxiety.
- Support Groups: Online or local communities offer shared experiences and emotional validation.
- Mindfulness and Meditation: Practices that reduce stress and promote inner peace during an emotionally intense period.
- Education and Awareness: Understanding the science behind fertility options can reduce fear and bring clarity.
6.4 Talking to Partners and Family
Having open conversations with your partner or family about your fertility journey is crucial. Topics can include:
- Fertility goals and timelines
- Financial planning
- Emotional expectations
- Decision-making if IVF or frozen eggs don’t work
By addressing these early on, couples and families can feel more aligned and less emotionally strained during the process.
7. Financial Costs and Conscious Decision-Making
When considering egg freezing or IVF, financial readiness is a key factor. These treatments involve not just one-time procedures but also ongoing expenses.
7.1 Cost Breakdown (India-Based Estimates)
| Item | Approximate Cost (INR) |
| Fertility assessment tests (AMH, FSH, etc.) | ₹5,000 – ₹10,000 |
| Egg freezing procedure (per cycle) | ₹1,50,000 – ₹2,50,000 |
| Hormonal injections | ₹50,000 – ₹80,000 |
| Annual storage of frozen eggs | ₹20,000 – ₹50,000 |
| IVF with frozen eggs (future use) | ₹2,50,000 – ₹4,50,000 |
Note: Costs vary based on clinic location, quality, and doctor expertise. International clinics, especially in the U.S. or Europe, can cost significantly more.
7.2 Insurance and Tax Benefits
- Most insurance providers in India do not cover elective fertility preservation.
- Some policies may include fertility treatments if deemed medically necessary (e.g. before chemotherapy).
- There are currently no tax exemptions specifically for fertility procedures, but certain medical expenses can be claimed under Section 80D (check with your CA).
7.3 Financial Planning Tips
- Start saving early if you’re considering egg freezing.
- Explore EMI options or financing plans offered by fertility clinics.
- Compare multiple clinics based on success rate and transparency, not just cost.
7.4 Conscious Decision-Making: Is Egg Freezing Right for You?
Before committing to egg freezing or IVF, ask yourself:
- Am I choosing this out of empowerment or fear?
- Do I have the financial, emotional, and physical bandwidth for this journey?
- Have I spoken to a fertility counselor or a trusted medical advisor?
- Do I understand that egg freezing is a chance, not a guarantee?
7.5 Alternatives to Consider
Depending on your values and timeline, alternatives include:
- Embryo freezing with a partner’s or donor’s sperm
- Adoption or surrogacy, especially if natural conception is medically challenging
- Egg donation, typically used in IVF if egg quality is poor
- Natural fertility enhancements, including acupuncture, nutrition, and yoga
7.6 Redefining Motherhood in the Modern World
Societal norms around parenting are evolving. Motherhood doesn’t have to look like the traditional timeline. Whether you choose to become a parent at 25 or 45 — through natural conception, IVF, surrogacy, or adoption — the most important factor is intentionality.
Women today have more choices than ever before, but with choice comes the responsibility to understand those options fully. Egg freezing and late pregnancy are tools — not mandates. Use them wisely.
8. References
To support the facts, statistics, and procedures outlined in this guide, here are credible sources and research-based links:
American College of Obstetricians and Gynecologists (ACOG)
Society for Assisted Reproductive Technology (SART) – IVF Success Rates
Centers for Disease Control and Prevention (CDC) – Pregnancy Complications
Conclusion: Empowered, Not Pressured
You are not running out of time. You are exploring your options. Whether you’re 28 and considering freezing your eggs or 38 and wondering about IVF, your timeline is uniquely yours.
Modern medicine has expanded the definition of fertility and given women more autonomy over their reproductive health. But ultimately, the best decision is one made with self-awareness, education, and emotional clarity.
Remember: Your body, your pace, your future.
If you found this guide insightful, consider sharing it with others who may be navigating the same decisions. Let’s create a culture where reproductive choices are informed, supported, and celebrated.