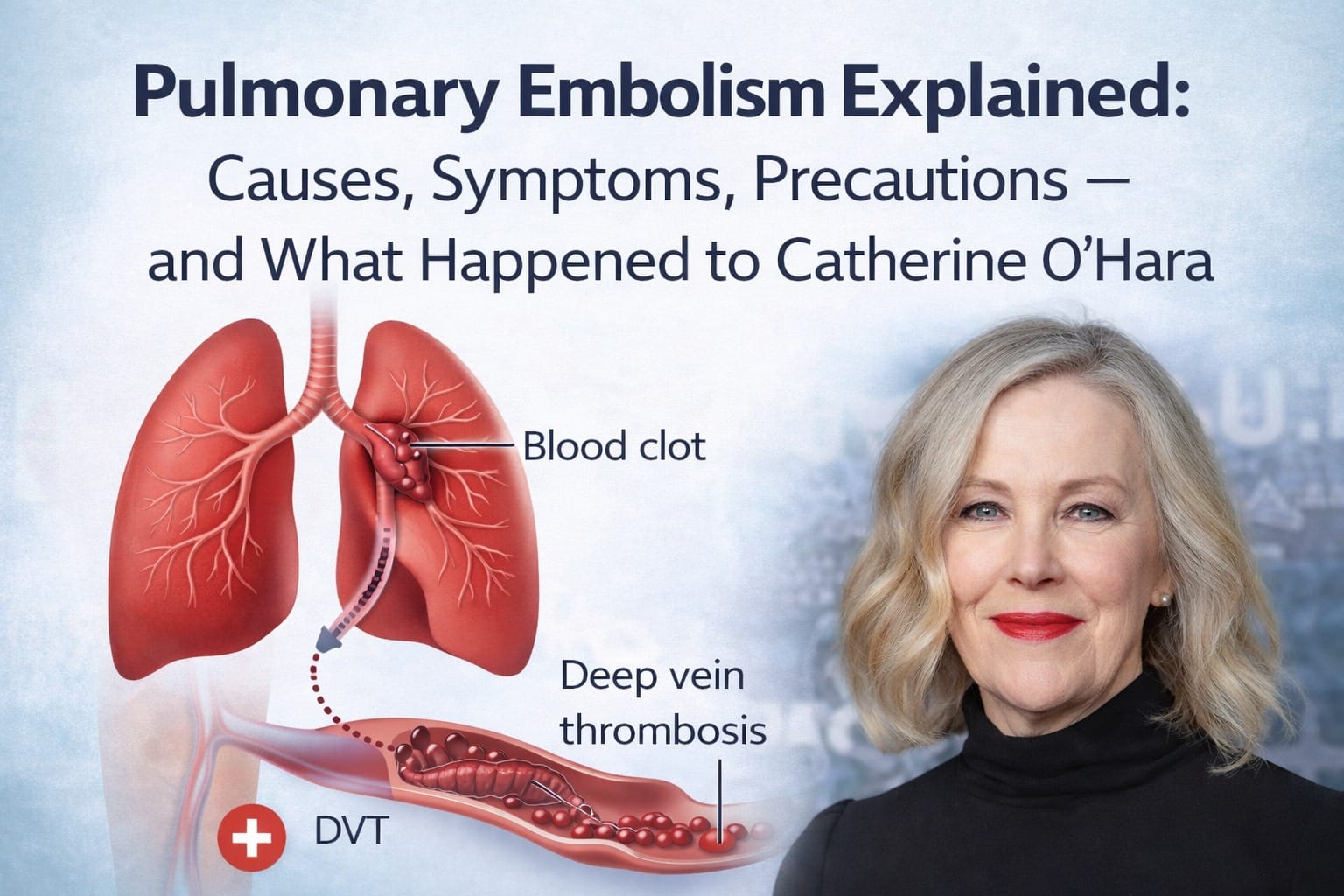
In February 2026, the entertainment world was shocked by the confirmed cause of death of beloved actress Catherine O’Hara — best known for roles in Schitt’s Creek and Home Alone. According to the Los Angeles County death certificate, the immediate cause of her passing on January 30, 2026, was a pulmonary embolism, with rectal cancer listed as an underlying condition.
But what exactly is a pulmonary embolism? Why does it occur? What are the symptoms, and how can it be prevented? This comprehensive article explains the condition in detail — from medical causes to risk factors and precautions — while tying in the real case of Catherine O’Hara’s tragic illness.
What Is a Pulmonary Embolism?
A pulmonary embolism (PE) occurs when a blood clot (or other material) travels through the bloodstream and blocks an artery in the lung, preventing normal blood flow. This blockage hinders oxygen exchange and can be life-threatening if not treated urgently.
Most pulmonary emboli originate from deep vein thrombosis (DVT) — blood clots that form in deeper veins of the legs or pelvis. When part of a DVT breaks loose and travels through the bloodstream, it can reach the lungs and cause a PE.
Although pulmonary embolism can affect people at any age, the risk increases with certain conditions, underlying health problems, or prolonged immobility. Without prompt treatment, even small clots can compromise lung function and cause rapid deterioration.
The Case of Catherine O’Hara: How It Happened
Catherine O’Hara died at age 71 on January 30, 2026, after being reported in serious condition and rushed to hospital. Her death certificate revealed that her immediate cause of death was a pulmonary embolism, a condition where a blood clot blocked blood flow to her lungs. Underlying this was her battle with rectal cancer, which can increase clotting risk.
Cancer, especially types like rectal cancer, increases the risk of blood clots because it can affect the way blood coagulates. Tumors and cancer treatments can trigger changes in blood clotting mechanisms, increasing the likelihood of clot formation.
In Ms. O’Hara’s case, while rectal cancer was the underlying condition, it was the pulmonary embolism caused by a traveling blood clot that directly led to her passing. The suddenness of PE is what makes it particularly dangerous — symptoms can develop quickly and may resemble other less serious conditions, making rapid medical response vital.
Also read – Why Intermittent Fasting can transform your life if done the right way
Causes of Pulmonary Embolism
1. Deep Vein Thrombosis (DVT)
The most common cause of pulmonary embolism is a blood clot that forms deep in the veins of the legs or pelvis — a condition known as DVT. When this clot detaches and travels through the bloodstream to the lung arteries, it causes a PE.
2. Prolonged Immobility
Sitting still for long periods — especially during long flights, extended bed rest, or recovery from surgery — slows blood flow in the legs. Slower blood flow increases the risk of clot formation.
3. Surgery or Major Injury
Major surgery, especially hip, knee, or abdominal surgery, increases the risk of blood clots because of prolonged immobility and changes in blood vessel walls.
4. Cancer and Cancer Treatments
Cancer, notably rectal or colon cancer, can disrupt normal blood clotting mechanisms. Chemotherapy and other cancer therapies may also raise the risk of DVT and subsequent PE.
5. Genetic and Blood Disorders
Certain inherited conditions (e.g., thrombophilia) make clotting more likely. People with these disorders are at higher risk of forming blood clots that can lead to PE.
6. Other Factors
Smoking, obesity, pregnancy, estrogen-based medications (like some contraceptives), and long-haul travel are common risk factors that contribute to clotting risk.
Symptoms of a Pulmonary Embolism
Pulmonary embolism symptoms can appear suddenly or develop over time. Because many symptoms overlap with other conditions, early recognition is crucial. Typical symptoms include:
- Sudden shortness of breath — the most common sign, especially when unrelated to exertion.
- Chest pain that may worsen with deep breathing or coughing.
- Rapid heart rate (tachycardia) and palpitations.
- Cough, sometimes with bloody or blood-streaked sputum.
- Dizziness or lightheadedness, potentially leading to fainting.
- Sudden unexplained fatigue and sweating.
In severe cases, a PE can lead to low blood oxygen, shock, or sudden death if the blockage is large or affects multiple lung arteries.
Diagnosing a Pulmonary Embolism
Accurate diagnosis requires medical evaluation and specific tests:
- Physical examination and history: Doctors assess symptoms and risk factors.
- D-dimer blood test: Elevated levels suggest clotting activity, prompting further testing.
- CT pulmonary angiography (CTPA): A detailed imaging test used to locate clots in the lungs.
- Ultrasound of legs: Checks for DVT clots in leg veins that might have traveled to the lungs.
- Ventilation/perfusion (V/Q) scan: Evaluates how air and blood are distributed in the lungs.
Prompt diagnosis is essential because delayed treatment increases the likelihood of complications.
Treatment Options
Treatment for pulmonary embolism aims to stop clot growth, prevent new clots, and restore blood flow:
Anticoagulants (Blood Thinners)
Medications such as heparin, warfarin, and newer oral anticoagulants reduce further clotting and help the body manage existing clots.
Thrombolytic Therapy
In severe cases, drugs may be used to actively dissolve clots. These are typically used when the risk to life is imminent.
Surgical Intervention
Rarely, surgery (embolectomy) is performed to physically remove large clots when other treatments fail.
Supportive Care
Oxygen therapy and monitoring in a hospital setting support breathing and circulation.
Precautions and Prevention
Preventing pulmonary embolism centers on reducing the risk of clot formation, especially in at-risk individuals:
Stay Active
Regular movement — especially during long travel or recovery — keeps blood flowing and reduces DVT risk.
Healthy Lifestyle Habits
Maintaining a balanced diet, managing weight, quitting smoking, and controlling chronic illnesses (like diabetes or heart disease) helps reduce clot risk.
Follow Medical Guidance
Use compression stockings during high-risk situations, take prescribed blood thinners when advised, and keep medical checkups up to date.
Post-Surgery Care
After surgeries, doctors often encourage early mobilization and, when appropriate, preventive anticoagulants to mitigate clot formation.
Early recognition of leg pain, swelling, or redness — potential DVT signs — can prompt early treatment and prevent progression to PE.
Final Thoughts
Pulmonary embolism is a serious medical emergency that requires swift diagnosis and treatment. Understanding its causes, symptoms, and risk factors can save lives. The tragic passing of Catherine O’Hara from a pulmonary embolism highlights how this condition — often silent until sudden — can affect even seemingly healthy individuals, particularly when underlying risk factors like cancer are present.
Being informed about warning signs and precautions is key to early intervention and prevention, especially for those with elevated risk. Regular health checks, active lifestyles, and timely medical care are essential components of pulmonary embolism prevention and management.
Disclaimer
This article is intended for general informational and educational purposes only. We are not medical professionals, and the content shared here should not be considered a substitute for professional medical advice, diagnosis, or treatment.
The information in this article has been compiled from trusted and credible public sources, including established news publications and medical reference platforms. While every effort has been made to ensure accuracy, readers are advised to consult qualified healthcare professionals for medical concerns or decisions.
If you or someone you know is experiencing symptoms related to pulmonary embolism or any medical emergency, please seek immediate medical attention.
Subscribe to our YouTube Channel The Logic Stick for more video insights